Headache or Migraine- What’s the Difference?
Most people know the feeling of pain and pressure in the head. Sometimes it starts slow and ramps up, other times it comes out of no where. And many of us know what to do about it: drink water, take NSAIDs, or lay down and sleep. For some, that means leaving work, missing school, passing on social opportunities and severe suffering.
The prevalence of head pain across the globe lead the International Headache Society to create a framework to assist in diagnosis and treatment of headache called the ICHD-2.
The International Classification of Headache (ICHD-2) Definitions
Head pain is divided into two categories: Primary headache and Secondary headache.
There are 4 types of primary headaches:
- Migraine Headache = no structural abnormality of brain on imaging
- Tension-Type Headache = neuronal dysfunction, poor modulation and central sensitization
- Trigeminal Autonomic Cephalalgias = Cluster Headache
- Other
Primary headaches are characterized as infrequent/episodic or chronic. Headaches are considered chronic when there are 15 or more days of pain in a month. Cluster headaches, on the other hand, are defined as less than 1 week absent of headache for more than 6 months.
On the flip side, secondary headaches, are acute and related to abnormalities on clinical examination. Dr. Vincent Martin from the University of Cincinnati created a mneumonic for screening secondary headaches that can be detected on physical exam.
The SNOOP mnemonic:
S: Systemic signs and symptoms
Fever, chills, weight loss, history of HIV or malignancy
N: Neurological signs and symptoms
Primary headache disorders have a normal neurological exam.
O: Onset
First and the worst headache of life. Headache that reaches peak intensity within seconds to minutes.
O: Older age
New onset of headache in someone after the age of 40. In general, primary headache disorders begin in young people.
P: Progression of an existing headache disorder
Change in location, quality, or frequency of the headache. The most common cause of this is medication overuse
Secondary headaches require intervention to address the underlying health condition before head pain can be addressed. A physical examination (including SNOOP) allows practitioners to rule out systemic causes of head pain. Interestingly, a very common cause of secondary headaches is visual deficits and referral to optometrist is usually required.

- ltimately, diagnosing headaches is symptom based and differentiated by frequency and chronicity.
- There are no true diagnostic studies used to rule in headache/migraine.
Let’s take a moment to get into some of the nitty-gritty around the cause of both headache and migraine.
Migraines
According to the Migraine Research Foundation, migraines are a neurologic disease affecting more than 39 million people in the U.S. and over 1 billion in the world.
Historically, migraines are thought to be related to vascular deficiency or poor blood supply. This remains unclear according to a 2014 study in NeuroScience which offers alternative etiologies. Such explanations include poor habituation (or adaptation) of cortical cells in the brain to non-noxious stimuli based on findings from several electrophysiological studies. Similarly, research is drawing a relationship between brainstem dysfunction and migraines. This theory assumes impaired regulation of descending inhibitory neural pathways.
What does this mean?
Simply put, it means that the brain over-reacts to everyday stimuli such as wearing glasses or your bra strap. The sensory input from the environment and everyday stimuli is poorly perceived and organized. When applied regularly (e.g. wearing a bra) the brain should recognize it as non-threatening and remember it. In cases of migraine, the brain fails to dampen to do that and results in excessive pain, or hyperalgesia. This phenomenon is called central sensitization.
Check out this video for a quick understanding of neuroscience
2 Minute Neuroscience: The Amygdala
What about headaches?
According to an article by Dr. Jennifer Kriegler, MD at the Cleveland Clinic, headaches have a lifetime prevalence of 30-78%. Mean onset occurs between 25 to 30 years old and a peak prevalence between age 30 to 39 years old.
Headaches often originate from pain activating structures in the head and neck. The most common source of head pain is muscular however that has not been fully supported in all studies. Interestingly, there is good data to support lifestyle and co-morbidities as a link to the experience of head pain. Common co-morbidities include TMD (tempromandibular joint dysfunction), depression, panic and anxiety attacks.
Interestingly, central sensitization seems to be a key player in the cause of headaches as well due to the relationship between myofascial dysfunction and sympathetic overdrive (excessive fight or flight).
[Read more about central sensitization from Dr. Sarah Crawford here.]
Another cause of head pain: Cervicogenic Headaches
Cervicogenic means referring from the cervical spine (or neck). Abnormalities in joint mechanics, soft tissue extensibility/pliability and stability are all culprits in referred pain to the head and neck. Further, we frequently see head pain coming from the upper back due to the coupling relationship between the thoracic and cervical spine.
Cervicogenic headaches are considered secondary headaches as they relate to underlying dysfunction.
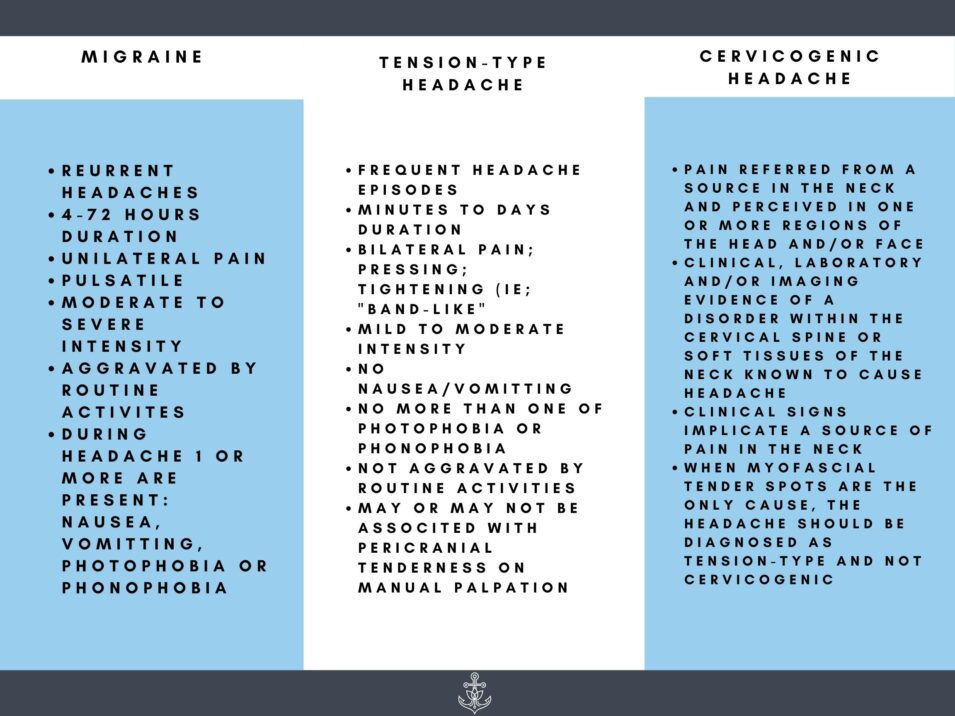
Symptom Differentiation
- Likely at this point you’re confused and overwhelmed.
- Below is a great table to refer to when trying to decide what you’re dealing with.
Can my headaches be treated?
Yes!
No matter if you are dealing with migraines, tension-type headaches, cluster or cervicogenic headaches, your pain can be treated. In most cases, there is a combination of each type of headache. It would be nearly impossible to have migraines without myofascial tender points.
Treatment focuses on addressing the underlying cause. Pharmacological interventions are sometimes necessary and likely include a cocktail of vasoconstrictive drugs like triptans and NSAIDs. Other common recommendations include electrolyte-based beverages, caffeine and water. Discussion around nutritional sensitivities plays an important role as dairy and wheat can often contribute to headache experience. Avoiding alcohol may also be beneficial, as many headache sufferers report alcohol as a trigger.
There does seem to be hope for migraine sufferers with relatively new FDA approved drugs like Aimovig, Ajovy and Emgality. In May 2019, the FDA approved the first wearable device Nerivio for the prophylactic treatment of migraines which is controlled with your smart phone.
Additionally, therapies including orthopedic manual therapy, acupuncture, trigger point dry needing, and massage are often useful. Evidence suggests that a strengthening program is often an integral piece of a program with the most robust long term benefits.
Speciality practice in treatment of headaches
In our practice, our treatment usually involves sympathetic down-regulating interventions to help decrease central sensitization. We work to improve the joint mobility of the cervical and thoracic spine. Myofascial trigger points and tender spots must be addressed with modalities such as massage, myofascial release, cupping and trigger point dry needling. We add stabilization and strengthening programs as the client begins to tolerate more activity without aggravation and can begin to self-manage symptoms.
We also address ergonomics, lifestyle choices, exercise and sleep hygiene as these will also contribute to onset of head pain. Lastly, we work closely with optometrist and visual therapist when occular deficits are involved due to the relationship between head pain and cervical dysfunction.
About the author:

Dr. Sarah Cash Crawford, PT, DPT, COMT, CMTPT, is a Physical Therapist and Certified Pilates Instructor. She has been a practicing physical therapy for over 10 years. With a background in neurologic rehabilitation, manual therapy and a specialty in treating chronic pain, Dr. Crawford has advanced training in orthopedic manual physical therapy and holds a certification in Geoffrey Maitland’s approach. She was also the first student certified by Myopain Seminars in Dry Needling, holding her Certified Myofascial Trigger Point Therapist credentials since 2014. Dr. Crawford studied Pilates early in her practice to further expand her treatment options to help patients overcome physical limitations. Dr. Crawford is the founder of the Anchor Wellness Center & Anchor Wellness, Inc., an integrated health and wellness collaborative.