Why Does My Back Hurt Every Day
1 out of every 2 people will experience low back pain at some point in their lives
I work out every day, I lift (heavy) weights, I do one million crunches for my core and I stretch every morning.
The internet is full of gadgets and gizmos promising to solve all your low back pain problems. But if that is the case, why is low back pain the second most common disability in the US? Depending on whom you ask, you will get a different answer. If you ask a podiatrist, they will usually blame your feet whereas many physical therapists will tell you your pelvis is “out of alignment.” Chiropractors, on the other hand, lean towards stiffness whereas personal trainers will identify core weaknesses.
Chronic low back pain is far more complicated than any of those answers
Consider these facts and statistics from the American Chiropractic Association:
- Worldwide, back pain is the single leading cause of disability, preventing many people from engaging in work as well as other everyday activities.
- Back pain is one of the most common reasons for missed work. One-half of all working Americans admit to having back pain symptoms each year.
- Back pain accounts for more than 264 million lost workdays in one year—that’s two workdays for every full-time worker in the country.
- Experts estimate that up to 80% of the population will experience back pain at some time in their lives.
- Back pain can affect people of all ages, from adolescents to the elderly.
- Back pain is the third most common reason for visits to the doctor’s office, behind skin disorders and osteoarthritis/joint disorders.
- Most cases of back pain are mechanical or non-organic—meaning they are not caused by serious conditions, such as inflammatory arthritis, infection, fracture, or cancer.
- Most people with low back pain recover, however, reoccurrence is common and for a small percentage of people, the condition will become chronic and disabling.
- Worldwide, years lived with disability caused by low back pain have increased by 54% between 1990 and 2015.
- Low-back pain costs Americans at least $50 billion in health care costs each year—add in lost wages and decreased productivity and that figure easily rises to more than $100 billion.
Back pain isn’t so simple.
More than likely, it’s a blend of everyone’s opinions. Research is not overwhelming for anyone intervention. Acupuncture, physical therapy, chiropractic, pharmacological or surgical. There is evidence to support and refute any of those options. Devices, exercises, sleeping positions– they all have their benefits– but alone, none are the answer.

What we can all agree on
Across the board, practitioners have become increasingly aware of the fact that chronic low back pain has a psychomotor component to it. What’s that mean? Psychomotor is the relationship between movement and conscious thought. Often, when we experience low back pain, we become fearful of it happening again. Our movements change as a result of experiencing pain in an effort to decrease the likelihood of feeling the discomfort again. Fear of moving then limits activity which eventually worsens your pain. Check out this Harvard Health article discussing the psychology of low back pain.
We know education is key.
Teaching individuals about the possible causes of pain and the best practices for working around pain are hugely important. Empowering individuals to modify not quit. Enlightening them on tools and tactics instead of abandoning and avoidance.
We also know that surgery is not indicated for back pain.
Surgery should only be considered when function (strength, range of motion, or sensation) is impaired to the extent that functional activities are limited. Many good neurosurgeons will tell you this. Oftentimes, though, someone will undergo back surgery and not experience any relief in pain. This is called “failed back surgery syndrome” and is likely the result of a poor understanding of the surgery. It’s a bit of a misnomer as the surgery didn’t fail. Likely, it corrected what it intended to correct (for example, removed a loose piece of disk material or stabilized a joint). Unfortunately, it just means that what was corrected was not the cause of the pain. Understanding the objectives of surgery is key.
Okay, so what can I do about my back pain?
First, start paying attention.
Bring your awareness to what you do on a daily basis. Pay attention to how you sit on the couch watching television. If you’re a man, think about whether or not you remove your wallet from your back pocket prior to sitting. For long-distance driving, notice whether your car has bucket seats that cause you to sit slumped or if you shift your weight more to one hip. Moms carrying babies tend to jut their hip out to the side. Often when standing, people shift their weight to one leg or the other. Do you suck your belly in or stick your butt out?
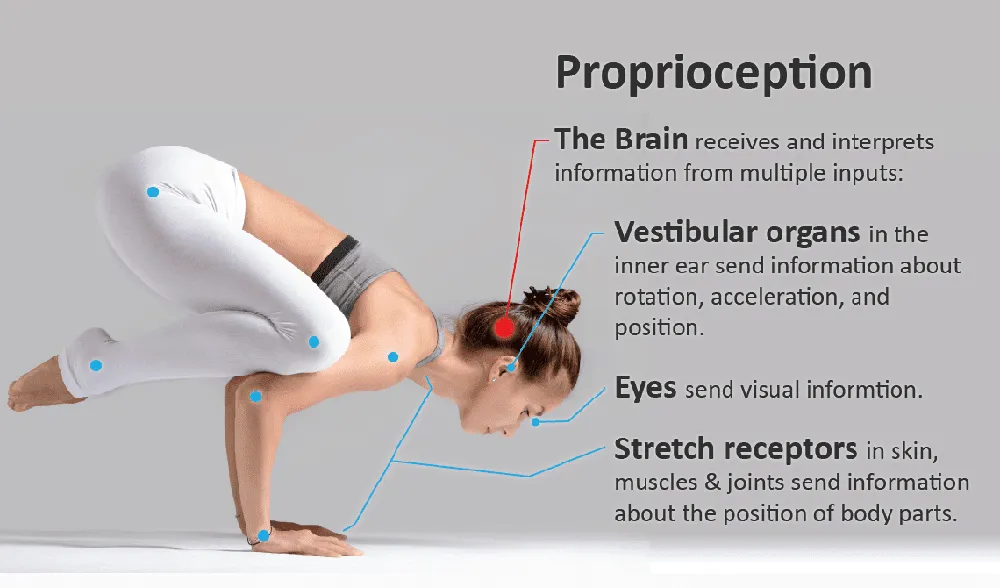
Kinesthesia
Bringing attention to our postures helps improve our kinesthetic awareness (or our knowledge of where our body is in space). We know that individuals with chronic low back pain have difficulty with visual imaging and proprioception and that improving those skills helps to diminish pain, as reported by La Touche et al in the Journal of Injury, Prevention and Rehabilitation.
Self-Efficacy
We also know that people need to believe that they can get better. This article by Arnes-Prieto et. al in Pain Physician demonstrates “that the level of self-efficacy not only affects the psychosocial sphere but can also interfere with physical performance and can even result in functional limitation.” That said, people who believe they can perform an activity have less pain intensity and disability when doing so.
Second, be willing to change.
If you identify something you’re doing on a daily basis aggravates your pain then you must be willing to change. Finishing every workout with 100 burpees may not be the best choice (I’ll poo-poo this even further in another blog in the future, stay tuned). Kettlebell swings are a good exercise when performed correctly but may not be helping you. Insisting on using your riding lawn mower when your daughter/son could do it may be problematic (check out this article about vibratory exposure and herniated disks).
Stress can be good but too much of it can be detrimental. If you recognize that you get tense during certain situations, then we have to identify tools to manage those times. An exercise is often a tool that people use to manage stress but as Dr. Solomon, PsyD posted in this blog post, too much exercise can sometimes have a negative impact on our mental health which unfortunately can propagate pain.
Third, be patient.
Your back pain didn’t start overnight and more than likely won’t resolve overnight. The wave of the future is utilizing a multi-disciplinary team to overcome back pain. The biopsychosocial model incorporates physical, social, and psychological factors when addressing disability and according to this systemic review by Guzman et al in BMJ, it’s been demonstrated that such intervention results in decreased pain and improved function for those with chronic low back pain.
Finding a team of providers who work together to help you strategize will optimize outcomes. Getting out of a silo-based approach will widen the view and enhance the outcomes.
What about acute low back pain after I workout?

If you’re one of the lucky ones who only experiences low back pain after you exercise then, unfortunately, you’re probably doing something wrong.
More than likely you don’t have the mobility/range of motion in your hips, knees, or ankles to execute a movement/exercise you’re doing or you don’t have intrinsic stability to offload additional resistance.
Our bodies are fantastically efficient machines.
If you decide you want to do something, the brain is all in. That said, it will go through the path of least resistance (ie; in a manner that requires the least amount of energy). If you’re lacking range of motion in your ankle, for example, you will make up for that somewhere else, like your HIP or BACK.
Try a few things of the following and take pictures/videos of yourself to get an idea of how you may be cheating:
- High plank- can you maintain a straight line from head to toe
- Sumo squat- are you shifting your weight or rotating to get depth
- High kneeling lunge- can you get your knee over your toes without your heel coming up?
- Pigeon pose- do you hyperextend through your low back
- Single knee to chest- can you get your knee past your hip (actively first, then passively
This isn’t a cure-all and the list above isn’t exhaustive. But it’s a good starting point. It provides an opportunity to gather data. Use it to get started and go from there.
About the author:

Dr. Sarah Crawford, PT, DPT, COMT, CMTPT, is a physical therapist and certified myofasical trigger point therapist through Myopain Seminars ®, the only certifying body of Trigger Point Dry Needling in the US. Dr. Crawford trained under Jan Dommerholt, PT and founder of Myopain Seminars ®, who worked directly under Drs. Travell and Simmons in his pursuit to bring dry needling to the U.S. Dr. Crawford has been performing Trigger Point Dry Needling in the Cincinnati area for over six years and was the first CMTPT in the state of Ohio. She has been practicing physical therapy for eight years. With a background in neurologic rehabilitation, manual therapy, and a specialty in treating chronic pain, Dr. Crawford began studying dry needling to further expand her treatment options to help patients overcome the influence of myofascial restriction. Dr. Crawford is the founder of the Anchor Wellness Center & Anchor Wellness, Inc., an integrative health practice that specializes in physical therapy and pilates.